

Arthroscopy is used to diagnose and treat lots of knee problems. Knee arthroscopy is a surgical procedure which let doctors view the knee joint without making a large incision through the skin and other soft tissues. The surgeon inserts a small camera, called an arthroscope, into your knee joint during knee arthroscopy. The procedure results in less pain for patients, less joint stiffness, and often shortens the time it takes to recover and return to favorite activities. Are you looking for Knee Arthroscopy Doctor in Ahmedabad? If yes then you are at the right place. Joint Care Arthroscopy Centre provides the solution for all kinds of knee arthroscopy diseases. We are expertise in Knee Surgery, Arthroscopic Surgeries, and Joint Replacement Surgery.
The proper functioning of the knee joint is vital for any human, it acts as a pivot joint which bond thigh and lower part of the leg and also enables the motion in the legs. Knee Arthroscopy is recommended if one has a painful condition that does not respond to nonsurgical treatment. Nonsurgical treatment includes physical therapy, rest, and medications or injections which can reduce inflammation.
Joint Care Arthroscopy Centre is the best centre in Ahmedabad offering facilities of minimally invasive orthopaedic surgery dealing with, Joint Surgery, Joint Replacement Surgery, Arthroscopic Surgery, Sports Surgery and Trauma Surgery using smaller incisions. With providing the best Knee Arthroscopy Doctor in Ahmedabad, the centre also facilities at the centre include splinting, Radiology, braces and all modern techniques of Physiotherapy with a fully equipped centre for sports injuries and their rehabilitation.
Maintaining a normal and active lifestyle with greater comfort is a key benefit of this procedure. Knee arthroscopy is an effective tool in treating your joint condition and for confirming treatment for knee problems like cartilage wear and meniscus tears. An arthroscopy can finally provide relief from knee pain and improve mobility.
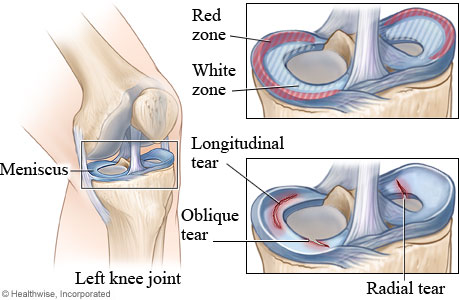
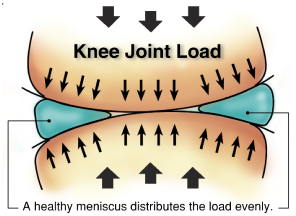
The cushion like shock absorbers present in the knee joint is called meniscus. There are two menisci in the knee. They sit between the thigh bone femur and the shin bone tibia. While the ends of the thigh bone and the shin bone have a thin covering of soft hyaline cartilage, the menisci are made of fibro cartilage and conform to the surfaces of the bones they rest on.
These menisci act to distribute body weight across the knee joint. Without the menisci, the weight of the body would be unevenly applied to the bones in the legs (the femur and tibia). This uneven weight distribution would cause the development of abnormal excessive forces leading to early damage of the knee joint. The menisci also contribute to the stability of the joint.
The two most common causes of a meniscal tear are traumatic injury (often seen in athletes) and degenerative processes, which are the most common tear seen in all ages of patients. Meniscal tears can occur in all age groups. Traumatic tears are most common in active people aged 10–55. Traumatic tears are usually radial or vertical in the meniscus and more likely to produce a moveable fragment that can catch in the knee and therefore require surgical treatment.
X-Ray during weight bearing can be obtained to rule out other conditions or to see if the patient also has arthritis. The menisci themselves cannot be visualised with plain radiographs. If the diagnosis is not clear from the history and examination, the menisci can be imaged with MRI scan. In straightforward cases, MRI will confirm or rule out the meniscus injury. Recent clinical data shows that MRI and clinical testing are comparable in sensitivity and specificity when looking for a meniscal tear.
The treatment course is dependent on the needs and status of the patient. A conservative course of treatment involving just physical therapy is possible. The patient will probably have to take a small break from his or her normal activities, allowing the knee to heal. Exercises can strengthen the muscles around the knee; especially the quadriceps which is longer and bigger muscle will protect the meniscus cartilage by absorbing a part of the weight. The patient may be given paracetamol or similar medication for pain. For patients with non-surgical treatment, physical therapy program is designed to reduce symptoms of pain and swelling at the affected joint. This type of rehabilitation focuses on maintenance of full range of motion and functional progression without aggravating the symptoms.
When conservative treatment fails or patients symptoms are persistent Arthroscopy is performed. In this procedure a key hole surgery is performed totrim the damaged meniscus or at times in repairable cases the meniscus is repaired. Arthroscopy is usually not recommended for a degenerative meniscus tear, unless there is locking or catching of the knee, recurrent effusion or persistent pain.
If the injury to the meniscus is isolated, then the knee would be relatively stable. However, if another injury such astorn ACL was coupled with a torn meniscus, then an arthroscopy would be performed. A meniscal repair has a higher success rate if there is an adequate blood supply to the peripheral rim. The interior of the meniscus is avascular, but the blood supply can penetrate up to about 6 millimetres. Therefore, meniscus tears that occur near the peripheral rim are able to heal after a meniscal repair. If the meniscus partially trimmed, the patient will be in rehab for about four to six weeks.
If a repair is conducted, then the patient will need four to six months. If physical therapy does not resolve the symptoms, or in cases of a locked knee then surgical intervention may be required. Depending on the location of the tear, a repair may be possible. In the outer third of the meniscus, an adequate blood supply exists and a repair will likely heal. Usually younger patients are more resilient and respond well to this treatment, while older, more sedentarypatients do not have a favourable outcome after a repair.

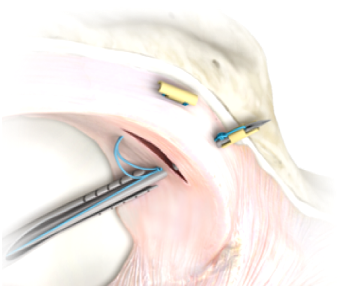
The meniscus has fewer vessels and blood flow towards the unattached, thin interior edge. In the majority of cases, the tear is far away from the meniscus’ blood supply, and a repair is unlikely to heal. In these cases arthroscopy allows for a partial meniscus trimming and allowing the knee to function with some part of the meniscus missing. Although its effects are not seen immediately, in long run of 10 15 years, the chances of the knee getting wear and tear in the articular cartilage is slightly increases compared with the normal knee.
After a successful surgery for treating the destroyed part of the meniscus patients must follow a rehabilitation program to have the best result. In most of the cases patient is discharged home same day in the evening partially weight bearing walking with the help of walker or crutches. They visit again at one week were dressing is removed and given home based physiotherapy instructions.
At 3 weeks post-surgery they are typically able to attend to 70 to 80% of normal daily activities, depending upon the procedure done at the time of surgery. At 6 weeks most of the patient are able to peruse their 95% of normal activities and are able to drive car and two wheelers. They are given specific restrictions depending upon their pathology found at the time of surgery.