

Patellar dislocation is a relatively common traumatic injury characterized by tearing of the connective tissue surrounding the knee cap (patella) with subsequent displacement ofthe patella so it is completely out of its normal position.
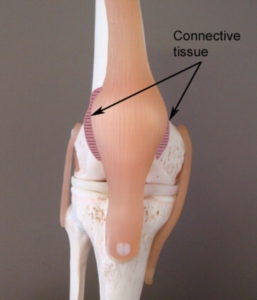
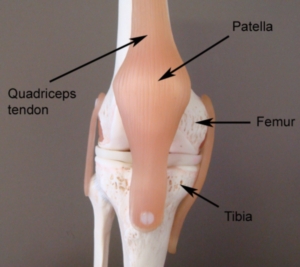
The knee comprises of the union of 3 bones – the long bone of the thigh (femur), the shin bone (tibia) and the knee cap (patella) (figure 1). The patella (knee cap) is situated at the front of the knee and lies within a groove at the front of the thigh bone. The tendon of the quadriceps muscle (the muscle at the front of the thigh) envelops the patella and attaches to the top end of the tibia (figure 1). Due to this relationship, the knee cap sits in front of the femur forming a joint in which the bones are almost in contact with each other. The surface of each bone, however, is lined with cartilage to allow cushioning between the bones. The patella also has strong bands of connective tissue known as the patella retinaculum (figure 2) attaching the knee cap on either side of the femur. This joint is called the patellofemoral joint.
Normally, the patella is aligned in the middle of the patellofemoral joint and is held firmly in place by the quadriceps muscle and patella retinaculum. Occasionally, the patella may be pushed completely out of its normal position. This normally occurs due to traumatic forces pushing the knee cap out of position beyond what the quadriceps and patella retinaculum-MPFL can withstand. When this occurs the condition is known as patellar dislocation.
Patellar dislocation usually occurs in a direction towards the outside of the knee (i.e. away from the other leg). During dislocation, tearing and disruption of the patellar retinaculum (Medial patellofemoral ligament) usually occurs. The joint surfaces may also be damaged and occasionally there may be an associated fracture. In many cases of patellar dislocation, the patella spontaneously moves back into its original position often with knee extension (i.e. straightening of the knee).
Patellar dislocation typically occurs when the forces pushing the knee cap out of its normal position are greater than the quadriceps muscle and patella retinaculum-Medial patellofemoral ligament can resist. This typically occurs traumatically due to excessive twisting or jumping forces or due to a direct blow (usually to the inner aspect of the patella). Occasionally, however, it may occur in the absence of trauma especially in young girls who are hyper-flexible. Patients with this condition are frequently seen in contact sports or sports requiring rapid changes in direction, such as football or rugby.
There are several factors which can predispose patients to developing this condition. These need to be assessed and, where possible corrected. Some of these factors include:
Patients with this condition usually experience sudden, intense pain at the front of the knee during injury. Pain is usually associated with a feeling of the knee ‘giving way’ or of something ‘popping out’. There may be a noticeable visible deformity of the knee owing to the knee cap moving out of position (normally to the outer aspect of the knee) when compared to the unaffected knee. There may also be a rapid onset of knee swelling within the first 1-2 hours following injury. In patients who have experienced recurrent episodes of patellar dislocation, the knee cap may easily move back into its original position with certain knee movements (normally straightening of the knee). In these cases, pain and swelling may also be relatively minimal.
Once the patella has returned to its original position following dislocation, patients usually experience an ache that may increase to a sharper pain with activity. Pain is typically experienced during activities that bend or straighten the knee particularly whilst weight bearing. Activities that frequently aggravate symptoms include going up and down stairs or hills, squatting, lunging, running, jumping or attempting to kneel. Pain typically increases on firmly touching the borders of the patellofemoral joint (i.e. along the patellar retinaculum – figure 2) There may also be an associated clicking or grinding sound when bending or straightening the knee. Patients may also experience episodes of the knee giving way or collapsing due to pain. In long standing cases, there may be evidence of quadriceps muscle wasting.
A thorough subjective and objective examination from a doctor is usually sufficient to diagnose patellar dislocation. Investigations such as X-ray, CT scan or MRI should usually be performed to assist with diagnosis and rule out other conditions, such as fractures or severe cartilage damage.
Despite appropriate physiotherapy management, some patients undergoing conservative treatment fail to improve or experience recurrent episodes of dislocation and subsequently require surgery for an optimal outcome. The majority of patients with severe cartilage damage or fractures also require surgery. Surgery for patellar dislocation is usually arthroscopic and typically involves removal of any loose bodies or torn cartilage and reconstruction of the torn patella retinaculum-medial patellofemoral ligament with moniopen technique. Usually a hamstring tendon is harvested and MPFL is reconstructed as shown in the figure.
Physiotherapy treatment for patellar dislocation is vital to hasten the healing process, reduce the likelihood of recurrence and ensure an optimal outcome. Treatment may comprise: